Introduction
Acne is one of the most common dermatological conditions worldwide, affecting adolescents and adults and often leaving psychosocial and physical scars. Whether you’re seeking fast acne treatment, long-term acne prevention, or evidence-based guidance for clear skin, this guide brings together up-to-date clinical recommendations, recent scientific findings, and practical skincare steps. Below you’ll find an SEO-friendly, medically grounded overview of acne causes, symptoms, types, and effective treatments, plus key points, an easy-to-read table, and citations to leading guidelines and peer-reviewed studies.
Key Points
- Acne is caused by a combination of excess sebum, follicular hyperkeratinization, microbial activity (Cutibacterium acnes), and inflammation. PubMed+1
- Clinical guidelines strongly recommend topical retinoids, benzoyl peroxide, and appropriate oral agents (including antibiotics and hormonal therapy) depending on severity; oral isotretinoin is the standard for severe, scarring, or treatment-resistant acne. PubMed+1
- Dietary patterns—particularly high-glycemic-load diets and some dairy consumption—can worsen acne in susceptible individuals; low-GI diets can help reduce severity in some studies. PMC+1
- The skin microbiome and strain-specific behavior of Cutibacterium acnes influence acne severity and are research priorities for new therapies. PMC+1
- Stress and hormones (e.g., cortisol, androgens) can exacerbate acne—stress management is a useful adjunct to medical therapy. PMC+1
What is Acne?
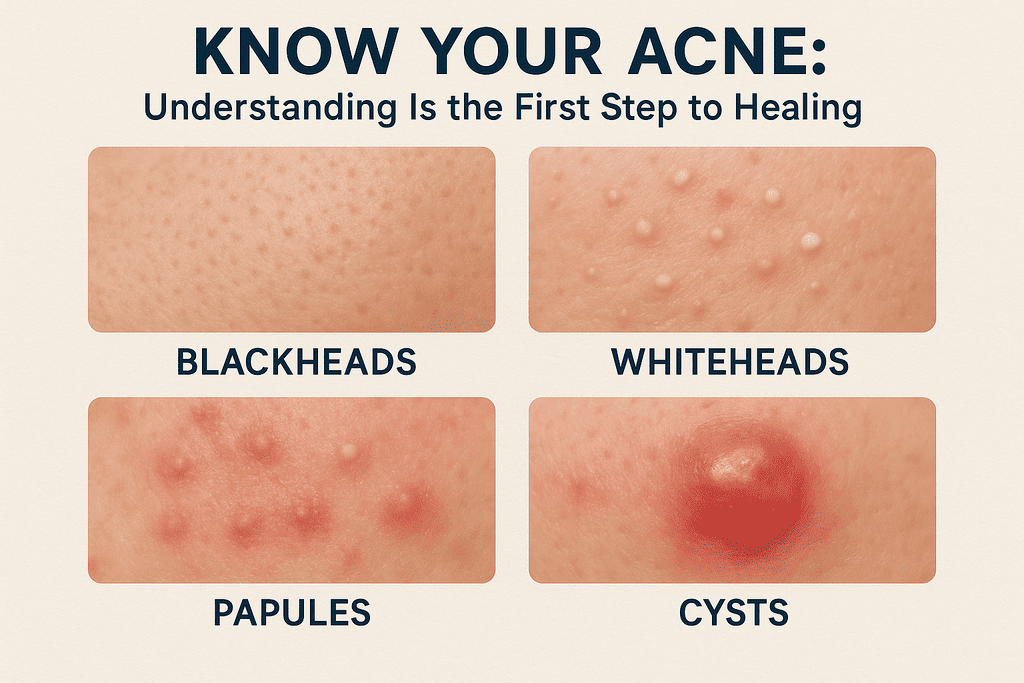
Acne vulgaris is a chronic inflammatory disease of the pilosebaceous unit characterized by comedones (blackheads & whiteheads), papules, pustules, nodules, and cystic lesions. While most prevalent during adolescence, acne also affects adults—particularly women—and can lead to permanent scarring and mental-health consequences. Clinical practice guidelines summarize the pathogenesis as a four-step process: increased sebum production, follicular hyperkeratinization, microbial colonization, and inflammatory responses. PubMed+1
Types and Severity of Acne (Table)
| Acne Type | Typical Features | Common Location | Treatment considerations |
|---|---|---|---|
| Mild Acne | Few comedones, occasional papules | Face | Topical retinoids, benzoyl peroxide |
| Moderate Acne | Multiple inflammatory papules/pustules | Face, chest, back | Topicals ± oral antibiotics or hormonal therapy |
| Severe/Nodulocystic Acne | Painful nodules, cysts, risk of scarring | Face, trunk | Oral isotretinoin or specialist care |
| Comedonal Acne | Dominated by blackheads/whiteheads | T-zone | Topical retinoids, chemical exfoliation |
| Hormonal/Adult Female Acne | Cheek and jawline dominant, cyclical flares | Lower face | Combined oral contraceptives, anti-androgens |
(Identifying the acne type is essential to choose the correct, evidence-based therapy.) PubMed
Signs & Symptoms
Common symptoms include :
- Open comedones (blackheads) and closed comedones (whiteheads).
- Red, tender papules and pustules that may be sore to the touch.
- Deep nodules or cysts that are painful and more likely to scar.
- Lesions most often appear on the face, upper back, chest, and shoulders.
Early recognition limits scarring and prolonged psychological impact. Seek dermatologist evaluation for painful nodules, widespread disease, or sudden changes in acne pattern. PubMed
Causes and Contributing Factors (Evidence-Based)
- Hormonal influences: Androgens increase sebum production; hormonal fluctuations are key in puberty, menstrual cycles, pregnancy, and certain endocrine disorders. Hormonal acne often responds to combined oral contraceptives or anti-androgen therapy. PubMed+1
- Genetic predisposition : Family history strongly predicts acne risk and severity.
- Microbial factors : Cutibacterium acnes (formerly Propionibacterium acnes) contributes to inflammation; recent work emphasizes specific strains and microbiome imbalance rather than mere presence/absence. PMC+1
- Dietary triggers : High-glycemic-load diets and certain dairy products have been linked to worse acne outcomes in multiple studies and meta-analyses; low-GI diets sometimes reduce lesion counts. Individual responses vary and a trial of dietary modification under professional guidance can be useful. PMC+1
- Stress and neuroendocrine factors : Stress elevates cortisol and can disrupt skin barrier and immune responses, promoting acne flares. PMC+1
- Topical and environmental factors : Heavy cosmetics, occlusive creams, sweat, and pollution can clog pores and aggravate acne.

Evidence-Based Treatments
First-line and topical therapies
- Topical retinoids (adapalene, tretinoin) — normalize keratinization and prevent comedones.
- Benzoyl peroxide — antibacterial and reduces risk of antibiotic resistance.
- Topical antibiotics (clindamycin) — useful in combination with benzoyl peroxide; avoid monotherapy to reduce resistance.
Clinical guidelines give strong recommendations for these agents in appropriate combinations. PubMed
Systemic therapies
- Oral antibiotics (doxycycline, minocycline) — for moderate inflammatory acne; use limited durations and combine with topical benzoyl peroxide. PubMed
- Hormonal treatments — combined oral contraceptives and antiandrogens (spironolactone) are effective for many women with hormonal acne. PubMed
- Oral isotretinoin — the most effective treatment for severe, nodulocystic, or scarring acne; requires specialist monitoring for side effects and pregnancy avoidance. Guidelines strongly support isotretinoin for severe or refractory acne. CNIB+1
Complementary and topical natural agents
- Tea tree oil has demonstrated efficacy in mild-to-moderate acne in randomized trials and recent systematic reviews, but concentration and formulation matter to avoid irritation. Frontiers+1
- Green tea extract, honey, and certain botanical agents show potential but should complement—not replace—evidence-based medical therapy. PMC
Emerging therapies & microbiome approaches
Research into microbiome-targeted treatments (strain-specific interventions, probiotics, bacteriophage therapy) is active; early studies suggest promising directions but more clinical trials are needed before routine use. PMC+1

Lifestyle, Skincare, and Prevention Tips
- Follow a gentle twice-daily cleansing routine with non-comedogenic products.
- Use oil-free, non-comedogenic cosmetics and sunscreen labeled not to clog pores.
- Avoid picking or squeezing lesions to reduce risk of scarring.
- Consider a low-GI diet trial and monitor for changes, especially if dairy or high-sugar foods seem to worsen flares. PMC
- Incorporate stress-reduction (sleep, exercise, mindfulness) into acne management plans. ScienceDirect
Short Answers
Q: Can diet really affect acne?
A: Yes—consistent evidence links high-glycemic-load diets and some dairy products to acne severity for susceptible people, though responses vary. PMC+1
Q: Is isotretinoin safe?
A: Isotretinoin is highly effective for severe acne but requires medical supervision for side effects and strict pregnancy prevention. Guidelines recommend it for severe or scarring disease. CNIB+1
Q: Will tea tree oil help my acne?
A: Tea tree oil can reduce lesion counts in mild-to-moderate acne, but may cause irritation; choose clinically tested formulations and patch-test first. Frontiers+1
Conclusion
Acne is a multifactorial, treatable condition. Combining evidence-based medical treatments with sensible lifestyle adjustments—dietary moderation, consistent skincare, and stress management—delivers the best outcomes. For moderate to severe acne or rapidly progressive disease, consult a board-certified dermatologist to create a personalized treatment plan that may include topical regimens, oral agents, or isotretinoin. Ongoing research into the skin microbiome and diet will continue to refine acne care; current clinical practice is guided by robust international guidelines and high-quality studies cited above. With early, appropriate care, most people achieve significant improvement and reduce the risk of permanent scarring.
Selected Recent Studies & References
- Reynolds RV, et al. Guidelines of care for the management of acne vulgaris. Journal of the American Academy of Dermatology (JAAD), 2024. PubMed+1
- Meixiong J, et al. Diet and acne: A systematic review. Nutrition Journal / PMC, 2022. PMC
- StatPearls. Isotretinoin. Pile HD, 2023. CNIB
- Dessinioti C, et al. The Microbiome and Acne: Perspectives for Treatment. PMC, 2024. PMC
- Borzyszkowska D, et al. Evaluation of Hormonal Factors in Acne Vulgaris. PMC, 2022. PMC
- Kairey L, et al. Efficacy and safety of Melaleuca alternifolia (tea tree) oil for… Frontiers in Pharmacology, 2023. Frontiers
- Meixiong J. Diet and acne: A systematic review (additional diet evidence). PMC, 2022. PMC
- Niedźwiedzka A. The Role of the Skin Microbiome in Acne: Challenges and… International Journal of Molecular Sciences, 2024. MDPI
- American Academy of Dermatology – Acne clinical guideline summary. Académie Américaine de Dermatologie+1