Introduction
Irritable Bowel Syndrome (IBS) is a common functional gastrointestinal disorder that causes symptoms such as abdominal pain, diarrhea, constipation, bloating, and excess gas. Understanding IBS—and how lifestyle, dietary choices, psychological therapies, and selected natural remedies can help—empowers patients to manage symptoms and improve quality of life. This article reviews evidence-based natural treatments and complementary therapies, integrates recent scientific studies from Asia, North America and Europe, and provides clear, SEO-friendly guidance for patients and clinicians. Key evidence and practical recommendations are cited from major clinical reviews and trials to help you make informed decisions. PMC+1gastrojournal.org
Key points
- Understanding IBS is the first step in effective symptom control.
- Dietary strategies (notably the low-FODMAP diet) show strong evidence of symptom reduction for many patients. PMC
- Psychological therapies such as Cognitive Behavioral Therapy (CBT) and other brain–gut behavioral treatments produce clinically meaningful improvements. gastrojournal.org
- Probiotics and some herbal remedies (e.g., peppermint oil) may benefit specific symptoms, though evidence and strain/compound specificity vary. gastrojournal.orgPubMed
- Exercise, yoga, and stress management are effective adjuncts and have been supported by studies from Asia, Europe and North America. PMCPubMedThe Washington Post

The condition : What is IBS and who is affected?
IBS is a chronic disorder of brain–gut interaction characterized by recurrent abdominal pain associated with altered bowel habits (diarrhea, constipation, or mixed). Symptoms vary by person and over time. While exact causes remain incompletely understood, a mix of gut-brain axis dysregulation, altered gut microbiota, visceral hypersensitivity, prior infections, genetics and psychosocial stressors are implicated. PMCMDPI
Who’s at higher risk? Women report IBS more often than men; individuals with a personal or family history of functional GI disorders, those with high life stress or anxiety, and people with post-infectious changes after GI infections are more likely to develop IBS. PMC
Symptoms to watch for
Common IBS symptoms include:
- Abdominal pain (relieved by defecation in many patients)
- Diarrhea (IBS-D), constipation (IBS-C), or mixed patterns (IBS-M)
- Bloating and excessive gas
- Nausea or early satiety in some patients
Recognizing symptom patterns helps tailor interventions (dietary, psychological, pharmacologic, or integrative).
Evidence-based natural and complementary approaches
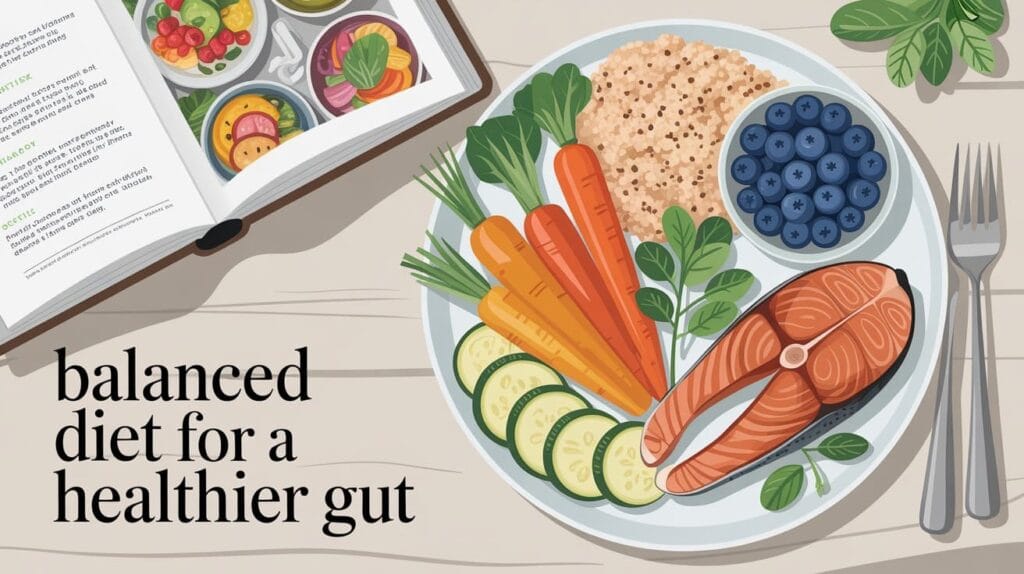
1. Dietary management — Low-FODMAP and personalized nutrition
A low-FODMAP diet (reducing fermentable oligo-, di-, mono-saccharides and polyols) is one of the most effective dietary interventions for IBS and should be implemented in phases (elimination, re-challenge, personalization) under the guidance of a trained dietitian. Randomized and systematic reviews report substantial symptom relief for many patients following a structured low-FODMAP program. American College of GastroenterologyPMC
Practical tips: keep a symptom-food diary, work with a dietitian to avoid unnecessary long-term restriction, and reintroduce foods to identify individual triggers. Hydration and regular meal timing also help regulate bowel habits.
2. Probiotics and microbiome-directed therapies
Some probiotics and specific strains demonstrate modest benefits for global IBS symptoms, bloating and stool regularity, but results are heterogeneous. High-quality meta-analyses caution that evidence certainty is low to moderate and effects are strain-specific—so pick products with clinical trial backing and discuss with your clinician. gastrojournal.orgPubMed
Note: Fecal microbiota transplant and emerging microbiome therapeutics are active research areas but are not standard therapies for routine IBS care outside trials. Wikipédia
3. Herbal remedies and nutraceuticals (peppermint, ginger, chamomile, turmeric)
Peppermint oil (enteric-coated) has repeatedly been investigated and may reduce abdominal pain and global symptoms in some trials; results vary across studies and formulations. Use caution with acid reflux or hiatal hernia because peppermint can worsen reflux in some people. PubMed+1
Other botanicals—ginger, chamomile, turmeric—have anti-inflammatory and digestive benefits supported by smaller trials and traditional use, but more rigorous RCTs are needed. Discuss herb–drug interactions with your clinician before starting supplements.
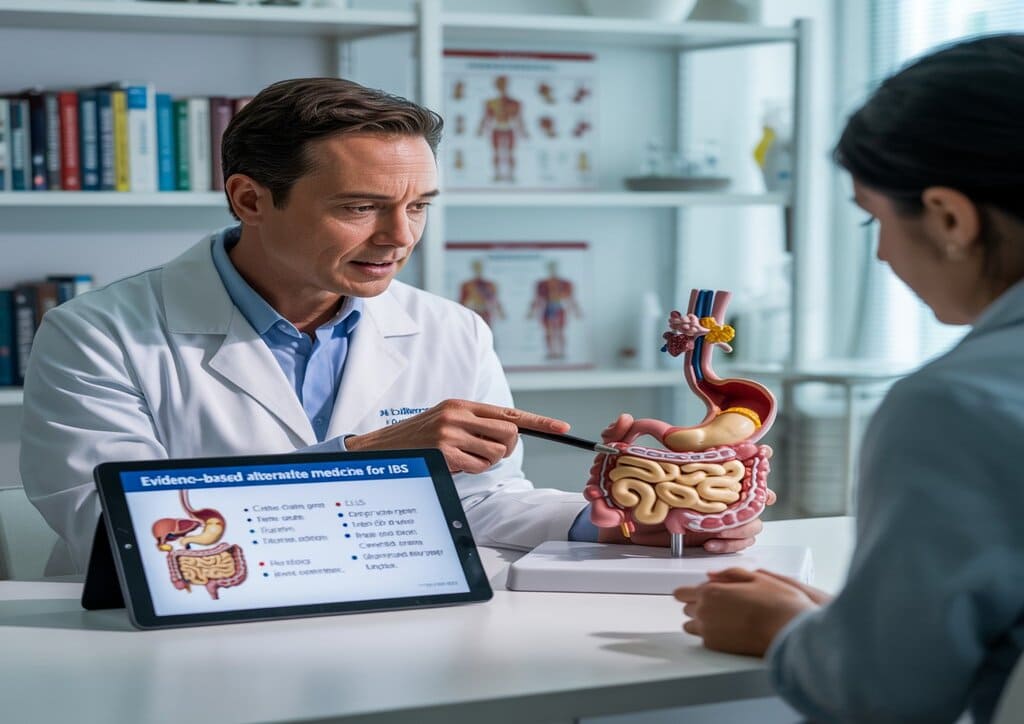
4. Brain–gut behavioral therapies : CBT, gut-directed hypnotherapy, mindfulness
Psychological approaches targeting the brain–gut axis, especially CBT, have demonstrated significant effectiveness in improving abdominal pain, bowel symptoms and quality of life. Recent multicenter analyses and gastroenterology reviews classified CBT and similar interventions as evidence-based options for moderate-to-severe IBS. gastrojournal.orgFrontiers
Delivery formats: individual therapy, group sessions, and digital CBT programs can be effective—choose what fits access and preference.
5. Exercise, yoga and stress-reduction techniques
Regular moderate physical activity and mind–body practices (yoga, meditative breathing) reduce symptom severity and improve wellbeing. A recent clinical study from King George’s Medical University (India) and subsequent trials reported that integrating yoga with standard care produced measurable symptom and anxiety reductions—important evidence from Asia supporting non-pharmacologic care. The Times of IndiaPMC
Safety, interactions and when to combine with conventional medicine
Natural and complementary therapies are adjuncts—not replacements—when symptoms are severe or red flags exist (weight loss, GI bleeding, persistent severe pain). Many patients benefit most from a multimodal plan that integrates dietary changes, probiotics or herbal agents (when appropriate), exercise, stress reduction, and, when needed, targeted medications. Always disclose supplements to your clinician to avoid interactions. The Washington Postgastrojournal.org

Figure / Table — Comparative effectiveness (summary of selected evidence)
| Intervention | Representative evidence & effect* |
|---|---|
| Low-FODMAP diet | Strong RCT & systematic review evidence — high symptom reduction for many patients. PMCAmerican College of Gastroenterology |
| CBT / brain-gut therapies | Randomized & meta-analytic evidence — improved pain and QoL. gastrojournal.orgFrontiers |
| Probiotics | Some strains beneficial; heterogeneity → low–moderate certainty. gastrojournal.org |
| Peppermint oil | Several RCTs show symptom improvement for abdominal pain in some patients. PubMed+1 |
| Yoga / exercise / stress reduction | Clinical studies (Asia, Europe, North America) report symptom and stress reduction. PMCPubMedThe Washington Post |
*Table is a summary—individual response varies; consult clinicians for personalized plans.
Practical, SEO-friendly patient checklist
- Get a clear diagnosis (rule out red flags).
- Start a symptom + food diary for 2–4 weeks.
- Consult a registered dietitian for a low-FODMAP trial if indicated. American College of Gastroenterology
- Consider a CBT referral or digital program for persistent pain/anxiety. gastrojournal.org
- If trying probiotics or peppermint oil, choose products with clinical evidence and track benefits. gastrojournal.orgPubMed
- Maintain regular moderate exercise and adopt stress-reduction practices (breathing, yoga, mindfulness). PubMedPMC
- Keep your healthcare team informed about supplements and symptom changes.
Conclusion
Managing Irritable Bowel Syndrome is often most successful when multiple evidence-based strategies are combined. Dietary modification (notably a structured low-FODMAP approach), psychological therapies (CBT and gut-directed treatments), targeted probiotics/herbal preparations, and lifestyle measures (exercise, yoga, stress management) form a pragmatic, patient-centered toolkit. Scientific research from Asia, Europe and North America continues to refine which combinations work best for different IBS subtypes; working with clinicians—gastroenterologists, dietitians and mental health therapists—ensures safe, tailored care. PMCgastrojournal.org+1
Selected References (key studies, reviews, guidelines and authoritative sources)
- Soufan F., The Gut-Brain Axis in Irritable Bowel Syndrome (review, 2025). PMC
- Goodoory VC., Efficacy of Probiotics in Irritable Bowel Syndrome (systematic review/meta-analysis, 2023). gastrojournal.org
- Kuźmin L., Efficacy of a Low-FODMAP Diet on the Severity (systematic review, 2025). PMC
- Gastroenterology journal / gastroenterology article on brain-gut behavioral treatments (2024). gastrojournal.org
- PubMed / randomized trials and reviews on peppermint oil for IBS (selected RCTs and meta-analyses). PubMed+1
- King George’s Medical University yoga for IBS study (India, 2025; International Journal of Yoga / regional reports). The Times of IndiaPMC
- American College of Gastroenterology / Low-FODMAP guidance & patient resources. American College of Gastroenterology
- Harvard Health / consumer guidance on IBS management (overview article, 2024). Harvard Health
- Washington Post coverage summarizing dietary and lifestyle evidence (2025). The Washington Post