Introduction
Acupuncture — a core modality of Traditional Chinese Medicine (TCM) — has been practiced for thousands of years to relieve pain, rebalance the body’s systems, and support neurological recovery. In contemporary medicine, acupuncture is often used as a complementary therapy alongside conventional treatments for chronic pain, neurological disorders, and stress-related conditions. Modern clinical research has begun to clarify how acupuncture interacts with the nervous system, blood flow, and neurochemical signaling, making it a subject of growing interest across Asia, Europe, and North America. However, while evidence supports benefit in several areas, researchers emphasize careful interpretation and more high-quality trials for some indications. NCCIH+1
Body
How acupuncture is thought to work (clinical and physiological mechanisms)
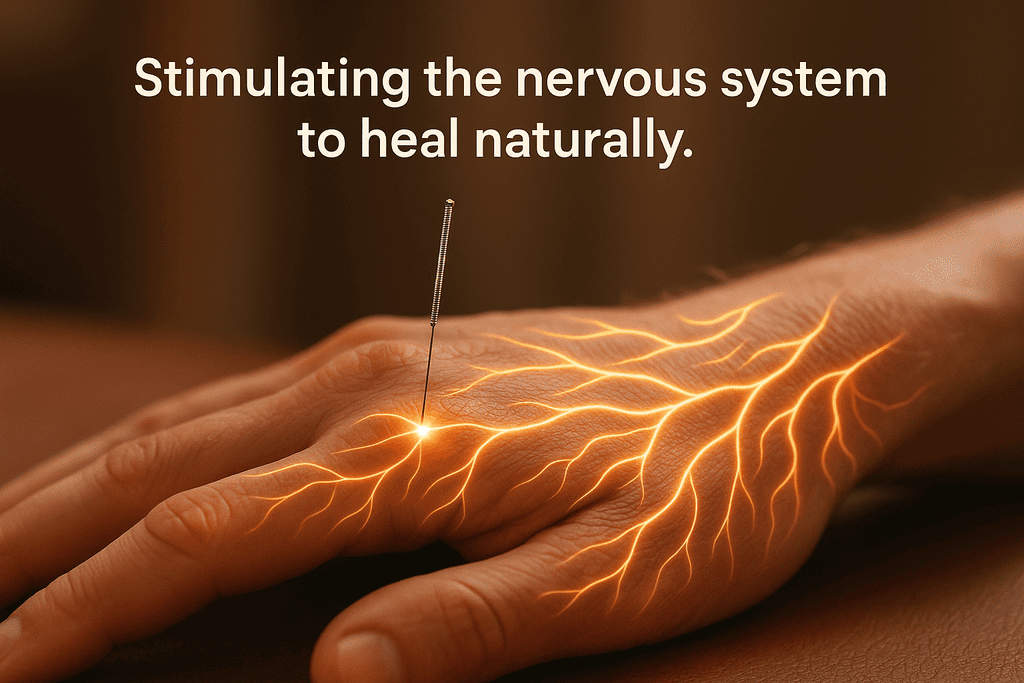
Acupuncture involves insertion of thin, sterile needles at specific anatomical points — commonly called acupoints — located along pathways known as meridians. From a biomedical perspective, needling appears to trigger a cascade of physiological responses: stimulation of peripheral nerves, modulation of spinal cord activity, release of endogenous opioids (endorphins), adjustments in serotonin and norepinephrine signaling, and localized increases in microcirculation and tissue oxygenation. These mechanisms may explain why acupuncture can reduce pain perception and influence autonomic and immune responses. Contemporary overviews from major institutions summarize these neurophysiological effects and encourage integrating acupuncture into multidisciplinary care where appropriate. NCCIH
Key Point: Acupuncture engages both peripheral and central nervous system pathways to modulate pain and physiological regulation. PubMed
Main clinical indications and levels of evidence
Research quality varies by condition, but several high-quality syntheses and randomized trials support acupuncture’s effectiveness in specific areas:
| Condition | Summary of Evidence / Typical Outcome |
|---|---|
| Chronic musculoskeletal pain (low back, neck, osteoarthritis) | Consistent evidence of pain reduction vs usual care; clinical superiority over sham is modest but reproducible. (IPD meta-analysis). PubMed+1 |
| Chronic headaches & migraines | Multiple RCTs and meta-analyses show reduced frequency and intensity; recommended as preventive option in several guidelines. PubMed |
| Neuropathic pain (including diabetic neuropathy, CIPN) | Growing evidence that acupuncture can reduce neuropathic symptoms and improve nerve conduction in some trials and meta-analyses, though larger multicenter RCTs are still needed. PMC+1 |
| Stroke rehabilitation & motor recovery | Systematic reviews suggest potential benefits for motor function when combined with rehabilitation, particularly in East Asian trials; evidence quality varies. ScienceDirect+1 |
| Parkinson disease (non-motor symptoms, sleep) | Emerging RCTs report improvement in sleep and some non-motor symptoms as adjunctive therapy; further replication required. JAMA Network+1 |
| Anxiety & insomnia | Several meta-analyses indicate positive effects on anxiety symptoms and sleep quality; acupuncture may be a useful adjunct. PubMed+1 |
Key Point : The strongest evidence currently supports acupuncture for chronic pain conditions (low back pain, neck pain, osteoarthritis, chronic headache) while evidence for neurological disorders is promising but still maturing. PubMed+1
Representative high-quality studies and international contributions
- Andrew J. Vickers et al. (United Kingdom / international) — A landmark individual patient data meta-analysis and updates have shown acupuncture is statistically superior to both usual care and sham acupuncture for chronic pain, with durable effects. This work is regularly cited as a central piece of evidence for acupuncture’s analgesic effect. PubMed+1
- World Health Organization (WHO) benchmarks and reviews (Global) — WHO and associated benchmark documents outline standardized training, safety practices, and a catalogue of conditions where acupuncture has evidence or historical use. These documents are important to policymakers and clinicians integrating acupuncture into healthcare systems. Organisation Mondiale de la Santé+1
- National Center for Complementary and Integrative Health (NCCIH) / NIH (USA) — Provides clinical summaries and guidance on safety, common uses (pain, headaches, osteoarthritis), and ongoing research funding for acupuncture trials. NCCIH
- Recent Asian and European trials — Large numbers of randomized and pragmatic trials from China, South Korea, Germany, and other countries have explored acupuncture for stroke recovery, diabetic neuropathy, chemotherapy-induced peripheral neuropathy, and Parkinson’s symptoms, adding region-specific expertise and methodologies. Several 2023–2025 meta-analyses and RCTs report positive findings but highlight methodological heterogeneity. ScienceDirect+2PMC+2
Typical treatment course, safety, and patient experience
A standard acupuncture session usually includes an initial assessment, gentle insertion of sterile single-use needles, and a rest period while needles are retained (commonly 15–30 minutes). Most patients report feelings of relaxation, warmth, or a mild “tingling” near insertion sites. Serious adverse events are rare when performed by trained practitioners; minor side effects (transient soreness, minor bleeding, bruising) occur occasionally. WHO and national bodies recommend accredited training and standardized safety protocols. Organisation Mondiale de la Santé+1
Key Point : Acupuncture is generally safe when performed by qualified professionals following infection-control standards. Organisation Mondiale de la Santé+1
Practical guidance for patients and clinicians
- Seek licensed or certified acupuncturists with relevant training and good clinical hygiene. Organisation Mondiale de la Santé
- Consider acupuncture as an adjunct — not a replacement — for evidence-based conventional care, especially for serious neurological conditions such as stroke or Parkinson’s disease. ScienceDirect+1
- Track progress with validated outcome measures (pain scales, sleep quality indices, neurologic function tests) and coordinate care across specialties. NCCIH
Figure (Suggested for web or print)
Figure 1 — Evidence Map : Acupuncture Indications and Strength of Evidence
(Visual idea for designers : a 3-tier chart — Strong Evidence (chronic pain, migraine), Moderate Evidence (neuropathic pain, insomnia), Preliminary / Emerging (stroke motor recovery, Parkinson’s non-motor symptoms). Use icons for pain, brain, sleep, nerves.)
Conclusion
Acupuncture sits at the intersection of ancient wisdom and modern science. Strong, consistent evidence supports its role in treating certain chronic pain conditions; growing international research suggests beneficial roles in neuropathic symptoms, stroke rehabilitation, and adjunctive support for neurodegenerative disorders, though higher-quality trials are still needed in several areas. Patients and clinicians should view acupuncture as a safe, evidence-informed complementary therapy when delivered by trained practitioners and integrated into multidisciplinary care plans.
Final Key Points
- Bold keyword : Acupuncture — effective for many types of chronic pain and promising for neurological support. PubMed
- Bold keyword : Neuropathic pain — emerging evidence supports benefit in diabetic neuropathy and chemotherapy-induced neuropathy. PMC+1
- Bold keyword : Safety — low risk when performed by qualified professionals; follow WHO and national benchmarks. Organisation Mondiale de la Santé
References and Selected Sources
- Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: update of an individual patient data meta-analysis. J Pain. 2018. PubMed+1
- World Health Organization. WHO benchmarks for the practice of acupuncture. 2021. Organisation Mondiale de la Santé
- National Center for Complementary and Integrative Health (NCCIH). Acupuncture: Effectiveness and Safety. NIH. NCCIH
- Hoerder S, et al. Acupuncture in diabetic peripheral neuropathy: systematic review and meta-analysis. 2023. PMC
- Yan M, et al. Acupuncture and Sleep Quality Among Patients With Parkinson Disease: Randomized Clinical Trial. JAMA Network Open. 2024. JAMA Network
- Huang S, et al. Acupuncture for acute ischemic stroke: systematic review and meta-analysis. 2024. ScienceDirect
- Mayo Clinic. Acupuncture — Overview. 2024. Mayo Clinic
- BMJ Open, Frontiers in Neurology, and other 2023–2025 reviews on acupuncture in neurological rehabilitation and non-motor symptoms (see individual articles cited in text). BMJ Open+1