Introduction
Late summer sliding into early autumn brings a distinct mix of heat, humidity shifts, airborne allergens, and respiratory viruses—all of which can nudge our bodies out of balance. The good news: most of these seasonal stressors are predictable and preventable with simple, evidence-based steps. This comprehensive guide explains the key health risks of late August through October, how to recognize them early, and what to do—grounded in recent research, medical guidance, and reputable references.
In this guide you’ll learn about:
- Heat-related illness during lingering late-summer heat waves and how to hydrate, cool, and acclimatize safely. JAMA NetworkCDCEPA
- Allergens that surge in late summer/early fall (ragweed pollen and mold), why symptoms spike in September, and treatment options. EPAAsthma & Allergy Foundation of AmericaMayo Clinic
- The “September asthma peak” and how to reduce emergency visits. Asthma & Allergy Foundation of AmericaPMCPubMed
- Mosquito-borne infections (especially West Nile virus) and practical bite-prevention. CDC+1
- Early-autumn respiratory viruses (flu, COVID-19, RSV) and optimal vaccine timing. CDC+1publichealth.jhu.edu
- Mood and sleep changes, including seasonal affective disorder (SAD), plus light-based strategies. WikipédiaMayo Clinic
Key Points
- Lingering heat in late summer remains a top risk; heat-related ER visits have increased in recent warm seasons. Plan cooling, hydration, and shade. CDC
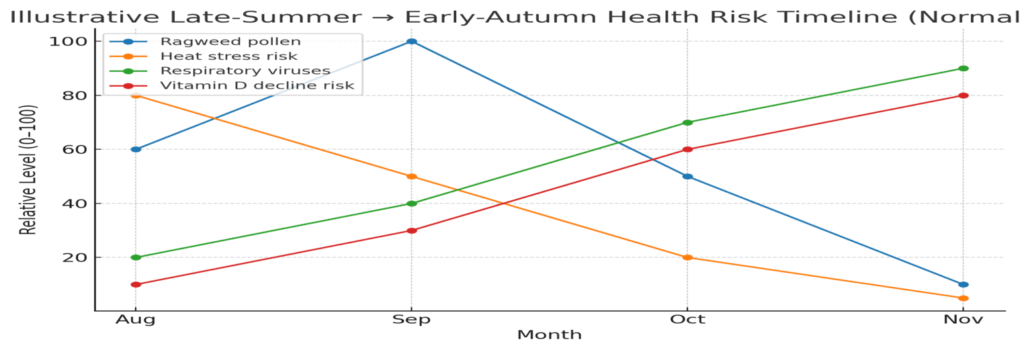
- Ragweed pollen peaks mid-September and mold spores rise with leaf fall and humidity swings—prime triggers for allergic rhinitis and asthma. Asthma & Allergy Foundation of America+1
- The third week of September is often “Asthma Peak Week,” especially for school-age children; step up controller meds per your action plan. Asthma & Allergy Foundation of America
- West Nile virus risk remains highest in late summer and early fall; use EPA-registered repellents and remove standing water. CDC+1
- Flu shots are best for most people in September–October; follow current guidance for COVID-19 updates. CDC+1
- Watch for SAD emerging with shortening days in early autumn; morning light, movement, and routine support mood. WikipédiaMayo Clinic

The Late-Summer Heat Problem (and How to Fix It)
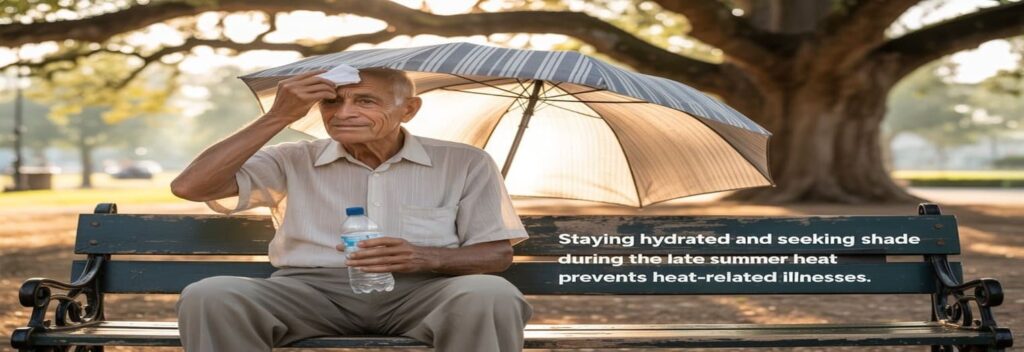
By late summer, heatwaves can still push body temperature and cardiovascular strain too far. A 2024 JAMA analysis shows heat-related mortality rates have risen from 1999–2023, with the sharpest increases in recent years—underscoring why late-season heat vigilance matters. Public health data also document surges in heat-related emergency visits during May–September. JAMA NetworkPMCCDC
Prevention
- Hydrate proactively: aim for pale-straw urine; pair water with electrolytes during heavy sweating.
- Cool strategies: shade, breathable clothing, fans with cross-ventilation, cool showers, and scheduled rest breaks.
- Time your activity: plan workouts in the cooler morning or evening; acclimatize gradually.
- Check meds: diuretics, anticholinergics, and some antihypertensives can affect thermoregulation—confirm with your clinician.
Treatment (mild heat illness)
- Move to a cool place, loosen clothing, sip fluids, and actively cool (cool cloths/ice packs in armpits/groin).
- Warning signs of heat stroke (confusion, fainting, very high body temp) require emergency care immediately.
Why this still matters in September: Persistent heat contributes to excess deaths even when not labeled as “heat stroke,” raising risks of cardiac and respiratory mortality. EPA

Allergens of Early Autumn : Ragweed and Mold
Ragweed pollen (a prolific weed allergen) peaks in late summer/early fall and can persist until the first frost. The U.S. EPA notes a lengthening of pollen seasons, and allergy organizations pinpoint mid-September as the typical high. EPAAsthma & Allergy Foundation of America
Mold spores flourish as nights cool, humidity fluctuates, and fallen leaves collect moisture. Exposure can trigger rhinitis and asthma flare-ups; reputable clinical sources emphasize vigilant control for people with mold-induced asthma. Asthma & Allergy Foundation of AmericaMayo Clinic
Prevention & Treatment
- Pollen strategy: track daily counts; keep windows closed on high-count days; use HEPA filtration indoors; shower after outdoor time; wear wrap-around sunglasses and a brimmed hat.
- Medications: start intranasal corticosteroids 1–2 weeks before your typical symptom onset; add non-sedating antihistamines and saline rinses as needed.
- Mold control: keep indoor RH 40–50%, fix leaks, vent bathrooms/kitchens, and promptly remove damp leaf piles; consider N95 during yard cleanup if you’re sensitive.
- Asthma action: review your written asthma plan; ensure inhaler technique; have rescue meds accessible and consider a step-up in controller therapy during high-trigger weeks (with clinician guidance).
The September Asthma Peak
Epidemiologic studies have long described a post–back-to-school spike in asthma exacerbations—often about 2–3 weeks after Labor Day—associated with rhinoviruses, allergen exposure, and routine disruption. Advocacy and clinical data mark September as “Asthma Peak Month,” with the third week frequently the worst. PMCPubMedAsthma & Allergy Foundation of America
What to do now
- Mitigate school triggers: emphasize hand hygiene, up-to-date action plans on file, and quick access to relievers.
- Allergen control: wash bedding weekly in hot water; vacuum with HEPA; consider dust mite covers if indicated.
- Vaccines: see the next section—timely flu and COVID vaccines help reduce illness-driven exacerbations. CDC+1

Respiratory Viruses: Flu, COVID-19, and RSV in Early Fall
With school and indoor gatherings resuming, respiratory viruses rebound. Expert summaries from major academic centers highlight summer waves of COVID that stretch into autumn, while influenza vaccination timing remains crucial. For most people, September–October is the ideal time to get the flu shot; specific groups (e.g., some pregnant people, or young children needing two doses) may follow tailored timing. publichealth.jhu.eduCDC+1
Action checklist
- Vaccinate: Flu in September/October; follow local/CDC updates for 2024–2025 COVID-19 formulations and eligibility. CDC+1
- Layer defenses: stay home if sick, improve ventilation, consider masks in high-risk settings, and keep antivirals (per clinician advice) on your radar for early treatment. ABC News
- Back-to-school hygiene: handwashing, surface cleaning, and sensible symptom checks reduce class-to-home transmission. michiganmedicine.org
Mosquito-Borne Risks : West Nile Virus (WNV)
Although outdoor evenings feel cooler, mosquito exposure remains high into early fall. CDC guidelines emphasize that ~94% of U.S. WNV cases occur July–September, with the mid-July to late-August window especially intense. Prevention is therefore still essential in September. CDC
Practical prevention
- Use EPA-registered repellents (DEET, picaridin, IR3535, oil of lemon eucalyptus).
- Wear long sleeves/pants at dusk and dawn; repair screens; remove standing water (planters, gutters, buckets).
- Remember: 1 in 5 infected individuals develop symptomatic illness; a small fraction develop neuroinvasive disease. Seek care for severe headache, neck stiffness, confusion, or high fever. westnile.ca.gov
Mood, Sleep, and Seasonal Affective Disorder (SAD)
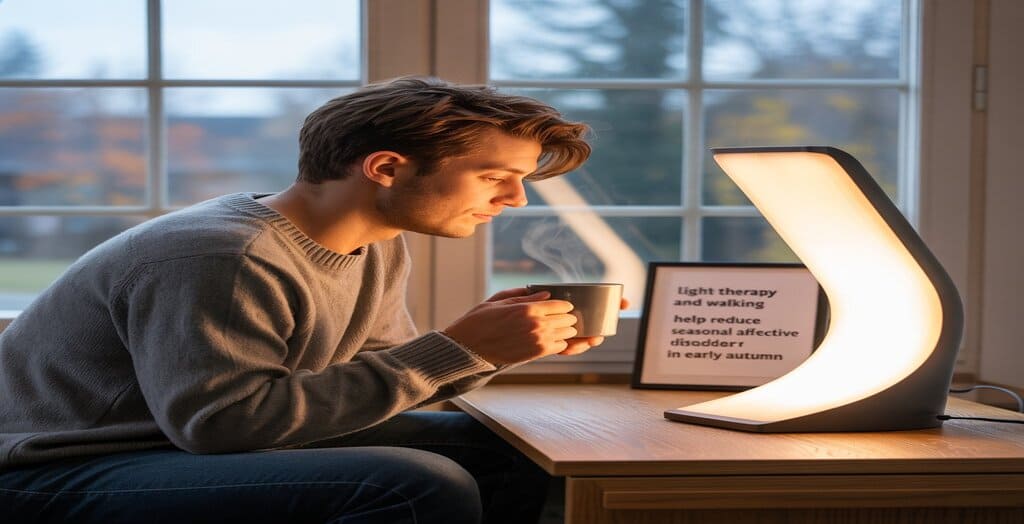
Shortening daylight can shift circadian rhythms, energy, and mood. Winter-pattern SAD often begins in late fall/early winter; staying proactive in early autumn helps. Wikipedia and clinical sources describe SAD’s pattern and management. WikipédiaMayo Clinic
What helps
- Morning light: daylight exposure within the first hour after waking; consider light therapy boxes (10,000 lux) after discussing with your clinician.
- Routine: keep consistent sleep/wake times, daily outdoor walks, and aerobic activity ≥150 minutes/week.
- Nutrition: emphasize produce, omega-3s, and adequate protein; discuss vitamin D status if at risk for deficiency.
- Reach out: cognitive-behavioral therapy and, in some cases, pharmacotherapy can be effective.
At-a-Glance Table: Seasonal Risks, Prevention, and First-Line Treatments
| Seasonal Issue | Typical Timing | Key Risks/Symptoms | Best Prevention | First-Line Treatments |
|---|---|---|---|---|
| Heat illness | Late Aug–Sept warm spells | Dizziness, cramps, confusion (severe) | Hydration, shade, timed activity, cooling plans | Cool environment, fluids/electrolytes; emergency care for heat stroke |
| Ragweed pollen | Aug–Oct (peak ~mid-Sept) | Sneezing, itchy eyes, congestion | Track counts, close windows, HEPA, shower after outdoors | Intranasal steroids, antihistamines, saline rinses |
| Mold spores | Early fall (leaf fall/humidity) | Rhinitis, asthma flares | Indoor RH 40–50%, fix leaks, yard cleanup | Environmental control; asthma action plan; meds per clinician |
| September asthma peak | 2–3 weeks after Labor Day | ER visits/exacerbations | Action plan at school, controller adherence | Step-up controller per plan; reliever access |
| WNV (mosquito) | Peak July–Sept | Fever; rare neuroinvasive disease | Repellent, clothing, drain standing water | Supportive care; urgent care for severe neuro signs |
| Flu/COVID/RSV | Sept–Nov upswing | Fever, cough, wheeze; exacerbations | Vaccines, ventilation, stay-home-when-ill | Antivirals per clinician; fluids/rest |
| SAD | Late fall onset | Low energy, sleep/appetite changes | Morning light, activity, routine | Light therapy, CBT, clinician-guided meds |
Sources highlight timing and patterns for pollen, asthma peaks, WNV transmission, flu vaccination windows, and SAD onset. Asthma & Allergy Foundation of America+1EPAPMCCDC+2CDC+2Wikipédia
Evidence Spotlight: What Recent Research Says
- Heat and health: A 2024 JAMA study found rising heat-related mortality in the U.S. from 1999–2023, reversing earlier downward trends, aligning with CDC surveillance showing elevated heat-related ER visits during warm months. Practical implication: keep heat plans in place into September. JAMA NetworkPMCCDC
- Allergies and asthma: Late-summer ragweed and fall mold exposure are consistent drivers of rhinitis and asthma flares; advocacy and clinical guidance call out September as a high-risk month for asthma, with a well-documented post-school return spike. Asthma & Allergy Foundation of America+2Asthma & Allergy Foundation of America+2PMC
- Vector-borne disease: CDC WNV guidance confirms July–September as the highest-transmission period, validating late-summer mosquito precautions. CDC
- Vaccination timing: CDC advises that September–October are the best months for flu vaccination for most people; check local guidance for COVID-19 updates each season. CDC+1
- Seasonal mood changes: Authoritative summaries (NIMH; Wikipedia overview) note SAD often begins late fall—so start light, sleep, and activity routines in early autumn. nimh.nih.govWikipédia
Action Plan for Families, Athletes, and Older Adults
For families with school-age kids
- Allergy calendar: start nasal steroids before mid-September if pollen-sensitive; keep rescue inhalers accessible; give the school your asthma/allergy plan. Asthma & Allergy Foundation of America
- Virus playbook: flu shots in Sept–Oct; reinforce handwashing; keep kids home when febrile. CDC
For athletes and outdoor workers
- Smart scheduling: train at cooler hours; hydrate to plan; use work-rest cycles in heat.
- Allergen exposure: sunglasses/hat, post-workout shower, and HEPA filtration at home reduce symptom load.
For older adults and those with chronic conditions
- Heat and meds check: review diuretics/anticholinergics with a clinician; ensure access to a cooling space. JAMA Network
- Vaccinations: be first in line each September–October; ask about antivirals if at higher risk for complications. CDC
SEO-Friendly Terms to Use in Your Content (bolded for emphasis)
late-summer health, early autumn wellness, ragweed allergy prevention, mold allergy treatment, September asthma peak, heat illness prevention, West Nile virus precautions, fall flu shot timing, COVID-19 fall booster, seasonal affective disorder (SAD), back-to-school viruses, respiratory hygiene, indoor air quality (HEPA), hydration and electrolytes, sleep routine in fall
Mini Table: Vaccine Timing at a Glance
| Vaccine | Best Timing (Most People) | Notes |
|---|---|---|
| Influenza | September–October | Young children needing 2 doses should start earlier to finish before peak season. CDC |
| COVID-19 (seasonal update) | As recommended each fall | Follow current public-health guidance for the 2024–2025 formulation and eligibility. CDC |
Conclusion
The close of summer and the arrival of autumn bring predictable environmental shifts: residual heat, ragweed and mold, the back-to-school virus uptick, mosquito activity, and early signs of SAD for some. A few proactive moves—heat plans, allergy control, vaccination on time, mosquito prevention, and light/sleep routines—dramatically cut risk and keep you feeling your best.
If you or a family member have asthma, heart disease, pregnancy, or are older, consider a personalized plan with your clinician for September and October. A written checklist on the fridge—hydration, meds refills, HEPA filter maintenance, repellent by the door, and vaccine appointments—goes a long way toward a safer, healthier transition from late summer into fall.
References (selected)
- Heat & Mortality / ER Visits: Howard JT et al. JAMA (2024); CDC MMWR (2024); US EPA Climate Indicators. JAMA NetworkPMCCDCEPA
- Ragweed & Pollen Season: US EPA Climate Indicators; Asthma and Allergy Foundation of America (AAFA). EPAAsthma & Allergy Foundation of America
- Mold Allergy: AAFA; Mayo Clinic clinical overview. Asthma & Allergy Foundation of AmericaMayo Clinic
- September Asthma Peak: AAFA; Sears MR (review); Larsen K et al. (AnnalsATS). Asthma & Allergy Foundation of AmericaPMCPubMedatsjournals.org
- West Nile Virus (WNV): CDC Surveillance & Control Guidelines; California WNV program. CDC+1westnile.ca.gov
- Vaccination Timing: CDC Flu Vaccination Timing; Vaccine dosage/admin updates. CDC+1
- Seasonal Affective Disorder (SAD): Wikipedia overview; Mayo Clinic; NIMH. WikipédiaMayo Clinicnimh.nih.gov
Disclaimer
This article is informational and not a substitute for medical advice. For personalized care—especially if you have chronic conditions, are pregnant, or care for young children—consult a qualified healthcare professional.