Introduction
The transition from late summer to early autumn is a dynamic period for the atmosphere: temperatures begin to fall at night, diurnal temperature ranges (DTR) can widen, humidity patterns shift, and plant life (notably ragweed and other late-season pollen producers) releases large amounts of allergens. For public health, this seasonal transition is far from benign. It brings a cluster of respiratory, cardiovascular, allergic, and mental-health challenges — and sometimes a surge in communicable respiratory infections as people spend more time indoors. Understanding these patterns helps public-health planners, clinicians, and individuals prepare and respond effectively.
Keywords (SEO): late-summer, early-autumn, seasonal transition, temperature variability, ragweed pollen, respiratory infections, influenza, RSV, allergies, public health, mortality, climate change.
Main points (at-a-glance)
- Temperature variability between warm days and cooler nights increases in many regions during the late-summer → early-autumn transition and is associated with rises in respiratory and cardiovascular morbidity. The LancetScienceDirect
- Ragweed and other late-season pollens peak from August through October in many temperate regions, driving an increase in allergic rhinitis and asthma exacerbations. Asthma & Allergy Foundation of America+1
- Respiratory viruses (influenza, RSV, and seasonal increases in COVID-19 in some years) typically begin increasing in autumn, raising hospitalizations—public health agencies publish seasonal outlooks to guide vaccination and mitigation. CDC+1
- Mental health and extreme-weather stressors can worsen during transitional seasons (e.g., abrupt temperature swings, storm events), with associations reported between temperature variability and mental-health hospital visits. The Lancet
- Climate change is shifting timing and magnitude of these seasonal hazards (longer pollen seasons, altered virus seasonality, amplified temperature variability), complicating preparedness. ScienceDirectThe Lancet

Body
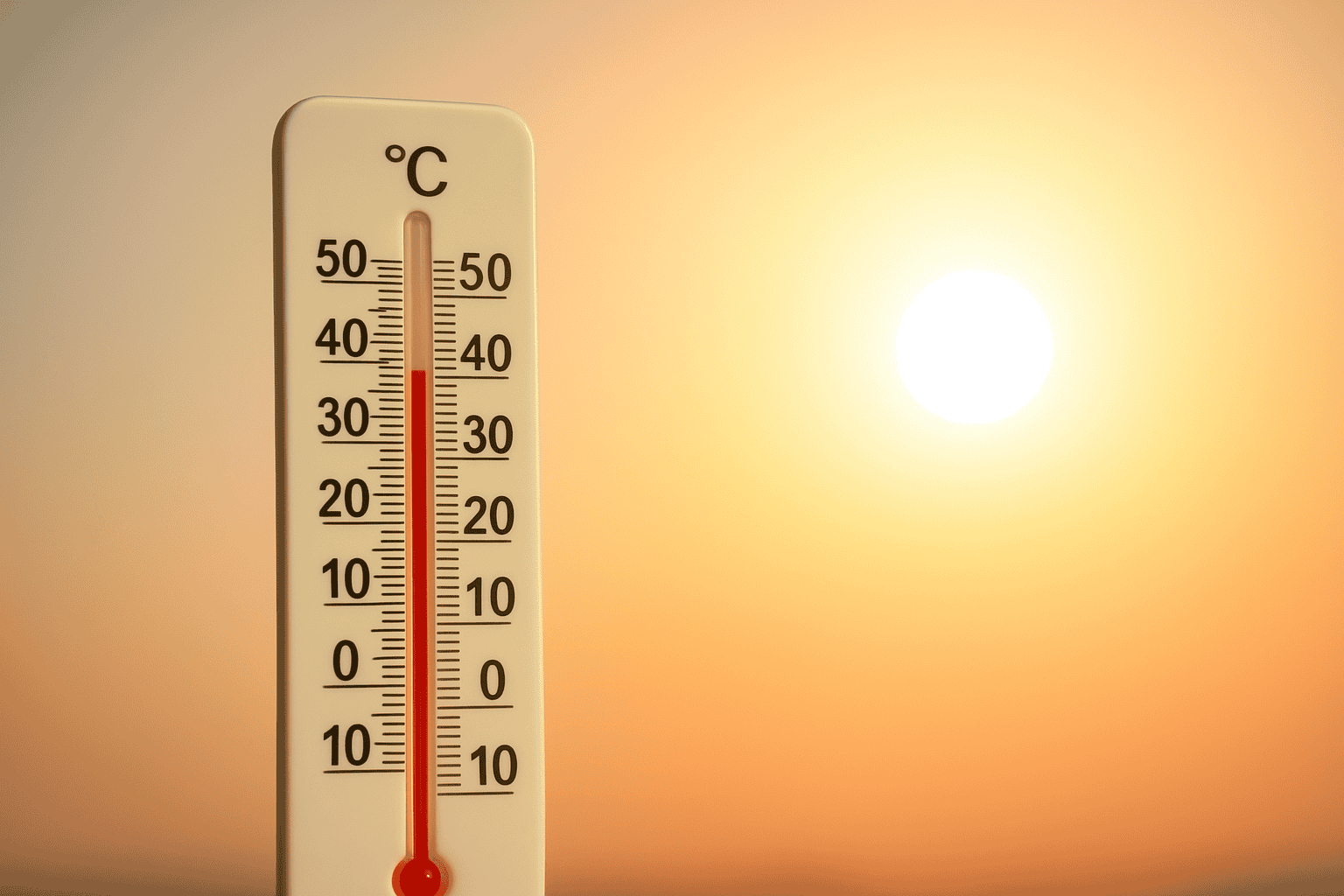
1. Meteorological features of the late-summer → early-autumn transition
Late summer and early fall are meteorologically active. Common features include:
- Widening diurnal temperature range (DTR) — warm daytime temperatures and cooler nights as radiative cooling strengthens. Studies link increased DTR to higher rates of respiratory and cardiovascular events. ScienceDirect+1
- Shifts in humidity and precipitation — some regions experience more convective storms or a shift toward drier air masses, affecting air quality and pollutant dispersion. Rainfall events themselves have been linked to short-term mortality patterns in large multi-location studies. BMJ
- Phenological changes — plants respond to accumulated heat and daylight changes; many late-season pollen producers (e.g., ragweed) release pollen when temperatures remain warm into August–October. Asthma & Allergy Foundation of AmericaScienceDirect
These atmospheric shifts create intersecting stresses for human health.
2. Respiratory infections: autumn is the beginning of “respiratory season”
Although respiratory viruses circulate year-round, many follow seasonal patterns. Influenza and RSV traditionally rise in autumn and peak in late fall/winter. Public health forecasting (e.g., CDC seasonal outlooks) advises vaccination campaigns and readiness for increased hospitalizations during this period. For example, the CDC has produced ongoing season outlooks for the 2023–2025 cycles and continues to monitor combined impacts of influenza, RSV, and COVID-19. CDC+1
Why autumn? Contributing factors include:
- Behavioral change (more time indoors, closer contact).
- Lower absolute humidity and cooler nights facilitating virus survival and transmission.
- Waning population immunity to particular viral strains and the annual “seeding” of local epidemics.
Clinically, this means health services should anticipate a rise in upper and lower respiratory tract infections, and vulnerable groups (infants, the elderly, immunocompromised) should be prioritized for vaccination and prophylaxis where available.
3. Allergies and asthma: ragweed and extended pollen seasons
Fall allergy season, driven mainly by ragweed in temperate zones, typically starts in August and often peaks in mid-September, continuing until first frost in many locations. Several authoritative summaries and allergy-capital reports show ragweed’s expanding season and range, likely linked to warmer temperatures and higher CO₂ levels that enhance plant growth and pollen production. The result: longer and sometimes more intense allergy seasons, which raise the risk of asthma exacerbations, increased clinic visits, and reduced quality of life for allergy sufferers. Asthma & Allergy Foundation of America+1
Practical public-health responses include forecasting pollen counts, encouraging patients with allergic rhinitis and asthma to keep medications handy (e.g., inhaled bronchodilators, corticosteroids, antihistamines), and using environmental controls (HEPA filters, limiting outdoor exposure on high-count days).

4. Temperature variability, cardiovascular risk, and mortality
Multiple large studies and meta-analyses indicate that non-optimal temperatures (both extremes and rapid variability) are associated with increased mortality and morbidity. A major global analysis estimated that millions of deaths are associated yearly with non-optimal temperatures, highlighting the public-health magnitude of temperature-driven risk. Additionally, intra-day and inter-day temperature variability appear to have differential effects on health outcomes, with some evidence linking higher variability during seasonal transitions to spikes in emergency visits for cardiovascular and respiratory conditions. The LancetScienceDirect
Mechanisms likely include physiological stress on the cardiovascular system (blood pressure fluctuations, increased cardiac workload), and on vulnerable populations such as the elderly and those with chronic cardiopulmonary disease.
5. Mental health and social implications
Temperature changes and extreme weather events can also affect mental health. Recent systematic reviews suggest associations between ambient temperature and mood disorders, emergency psychiatric presentations, and even suicidal behaviour in some settings. Late-summer heat waves followed by sharp cooling or storm events can create prolonged stress and disruption to routines, sleep patterns, and social supports — which adds to the disease burden during seasonal change. The Lancet

6. The role of climate change: shifting timing and intensity
Climate change is not simply warming — it is changing seasonality. Evidence shows that pollen seasons are lengthening, plant ranges are shifting, and the timing of first frosts is delayed in many regions, all of which extend the period of exposure to allergens. Climate shifts can also alter viral season timing and intensity by changing human behavior and environmental virus survival dynamics. This increases uncertainty for public-health planning and stresses the importance of year-to-year surveillance and adaptive responses. ScienceDirectThe Lancet
Prevention, preparedness and clinical recommendations
Individual-level actions
- Vaccination: get seasonal influenza vaccines and COVID/RSV vaccinations if eligible. Vaccination reduces severe disease and hospitalizations. CDC
- Allergy management: follow personalized asthma/allergy action plans, keep rescue medication available, monitor pollen forecasts, use HEPA filters indoors, shower after outdoor exposure. Asthma & Allergy Foundation of America
- Thermal regulation: wear layered clothing to adapt to diurnal swings, and avoid sudden exposure to cold nights after hot days.
- Hygiene & distancing: during peak respiratory activity, practice hand hygiene and stay home when sick to limit spread.
Health-system & public-health measures
- Seasonal surveillance: maintain robust respiratory surveillance and update seasonal outlooks (hospital capacity planning, vaccination timing). CDC
- Early-warning systems: pollen forecasts, heat/cold advisories, and temperature-variability alerts can guide personal and clinical preparedness.
- Targeted protection: proactively protect vulnerable populations (elderly, infants, chronic-disease patients) through outreach, vaccination clinics, and distribution of preventive tools.
- Climate adaptation: integrate changing seasonality into long-term health planning (extended allergy seasons, shifting vector-borne disease windows).
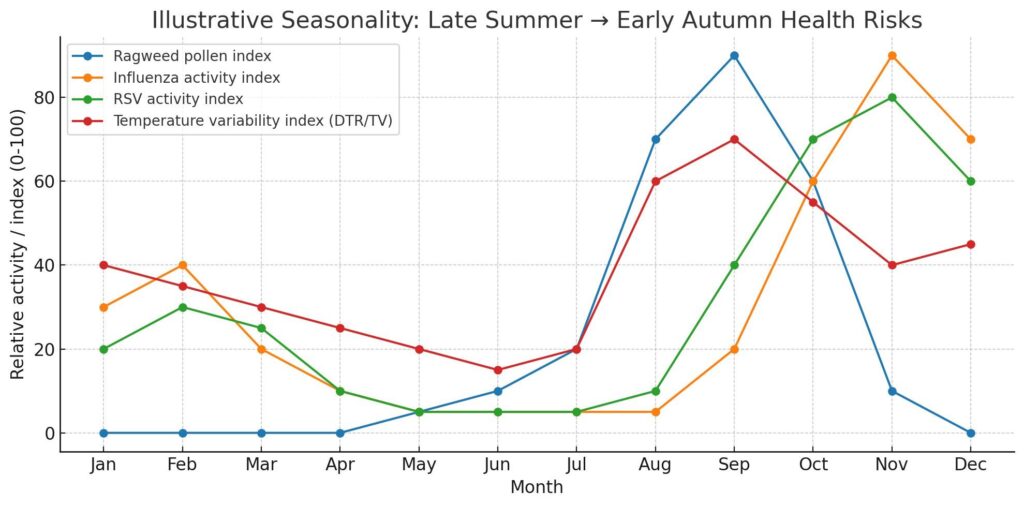
Charts and Visual Summary
I created an illustrative chart that overlays typical monthly activity for ragweed pollen, influenza, RSV, and a schematic temperature variability index to visualize the overlap of risk in late summer and early autumn. Download it here: Download the chart image.
Note: the chart is illustrative (schematic) — it synthesizes typical seasonal patterns drawn from surveillance and pollen reports and is meant to aid understanding, not to replace local forecasts. For local decisions, consult local health departments, pollen forecasts, and real-time surveillance.
Conclusion
The late-summer to early-autumn transition is a critical period for public health. Overlapping hazards — expanded pollen seasons, rising activity of respiratory viruses, and increased temperature variability — combine to raise the burden of allergic, respiratory, cardiovascular, and mental-health conditions. Climate change amplifies these trends and complicates planning. The best defenses are surveillance, timely vaccination, individual preparedness (medications, hygiene, thermal clothing), and adaptive public-health systems that incorporate changing seasonality into planning and communication.
Proactive measures taken in late summer — such as updating vaccination campaigns, educating at-risk patients, and issuing clear pollen and temperature-variability forecasts — can reduce hospitalizations, improve well-being, and make the autumn transition safer for vulnerable populations.
References & selected sources
(Selected recent or authoritative sources used to support key statements; not an exhaustive bibliography.)
- Global, regional, and national burden of mortality associated with non-optimal temperatures — The Lancet. The Lancet
- CDC Respiratory Illnesses Data Channel and 2024–2025 Respiratory Disease Season Outlooks — Centers for Disease Control and Prevention (CDC). CDC+1
- AAFA (Asthma and Allergy Foundation of America) — 2024 Allergy Capitals / ragweed season reports. Asthma & Allergy Foundation of America+1
- Systematic reviews on ambient temperature and mental health; temperature variability and health — The Lancet Public Health and related reviews. The LancetScienceDirect
- Seasonal virus dynamics and climate interactions — Lancet / EBioMedicine reviews on viral seasonality and climate change impacts. The LancetScienceDirect
- Multi-country studies on rainfall/temperature events and mortality — BMJ 2024 analysis. BMJ