Introduction
Obesity and overweight are global public-health challenges that affect millions of people and strain health systems worldwide. Over the past three decades, the prevalence of excess body weight has accelerated in nearly every region, with major consequences for cardiovascular disease, type 2 diabetes, certain cancers, and overall quality of life. Understanding what drives weight gain, how we measure risk, and which interventions work—backed by recent studies from leading researchers across Asia, North America, and Europe—is essential for individuals, clinicians, and policymakers. This article provides a comprehensive, SEO-optimized overview of the causes, health risks, and effective solutions for obesity and overweight, with key points, tables, and citations to authoritative medical and scientific sources.
Quick summary
- Obesity is defined by excess body fat that impairs health; BMI ≥ 30 is the commonly used threshold. (See BMI table below.) Organisation mondiale de la santé
- Global prevalence has risen sharply; over 1 billion people were living with obesity in 2022 according to large international analyses. Organisation mondiale de la santéReuters
- Major health consequences include heart disease, type 2 diabetes, certain cancers, and musculoskeletal disorders. AHA Journals
- Effective approaches combine balanced nutrition, regular physical activity, behavioral change, and, where appropriate, medical or surgical treatments. Recent clinical and population studies underscore multi-level solutions. The LancetPMC
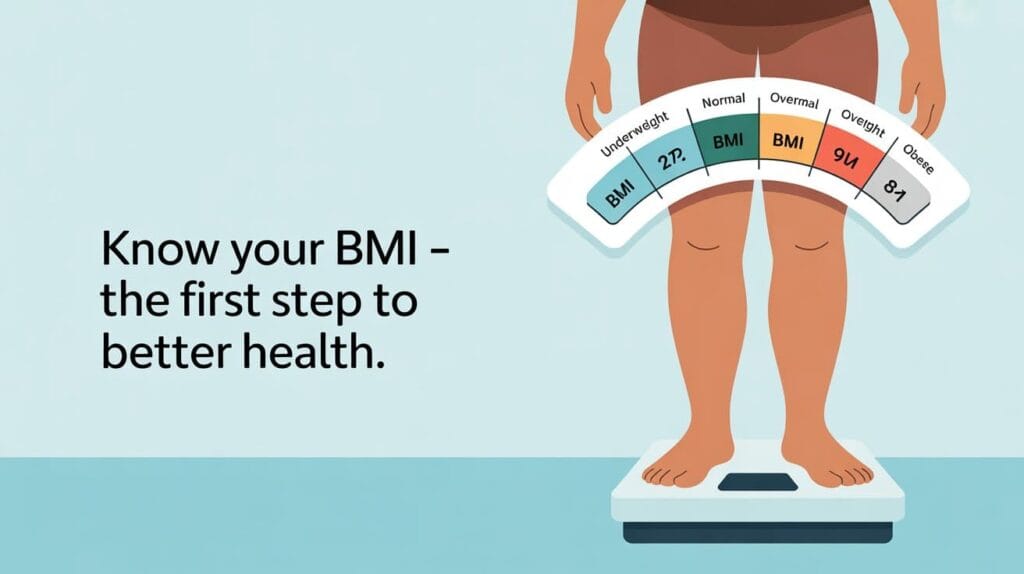
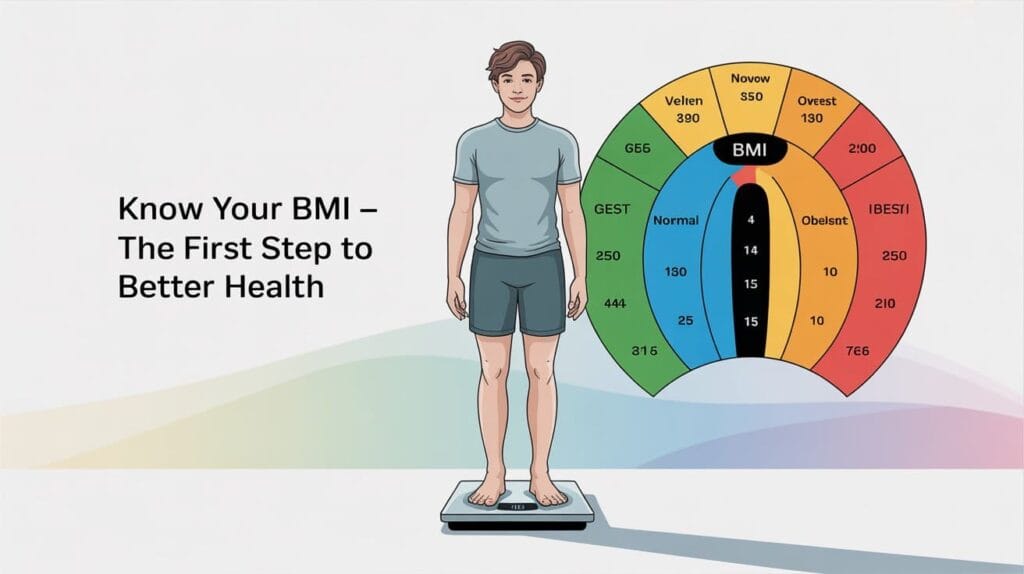
What is obesity? How is it measured?
Obesity is a chronic, relapsing medical condition characterized by excessive adipose tissue that impairs health. The most widely used screening tool is the Body Mass Index (BMI):
BMI = weight (kg) / height (m²)
Table 1 — BMI categories (standard WHO ranges)
| Category | BMI (kg/m²) |
|---|---|
| Underweight | < 18.5 |
| Normal weight | 18.5 – 24.9 |
| Overweight | 25.0 – 29.9 |
| Obesity (class I) | 30.0 – 34.9 |
| Obesity (class II) | 35.0 – 39.9 |
| Obesity (class III) | ≥ 40.0 |
Note: BMI is a population screening tool; waist circumference, body fat percentage, and clinical assessment give additional information about metabolic risk. Organisation mondiale de la santé

Why has obesity increased globally? Main causes and drivers
Obesity is multifactorial—driven by interactions between biology, behavior, the food environment, and social and economic factors. Key contributors include:
- Unhealthy diets: widespread availability of energy-dense, nutrient-poor processed foods and sugar-sweetened beverages.
- Physical inactivity: more sedentary jobs, mechanized transport, and screen time.
- Built environment & food systems: urban design, food marketing, and affordability shape choices. Recent systematic reviews identify the food environment as a key determinant of population weight trends. nutrition.bmj.com
- Biological and genetic factors: individual susceptibility, hormones, and metabolic differences.
- Socioeconomic and psychological factors: stress, sleep deprivation, and adverse childhood experiences influence eating and activity patterns.
Large global analyses and forecasting studies—led by multidisciplinary teams including researchers from Asia, Europe, and the Americas—show that trends reflect both individual behaviors and structural drivers that require policy-level responses. The Lancet+1
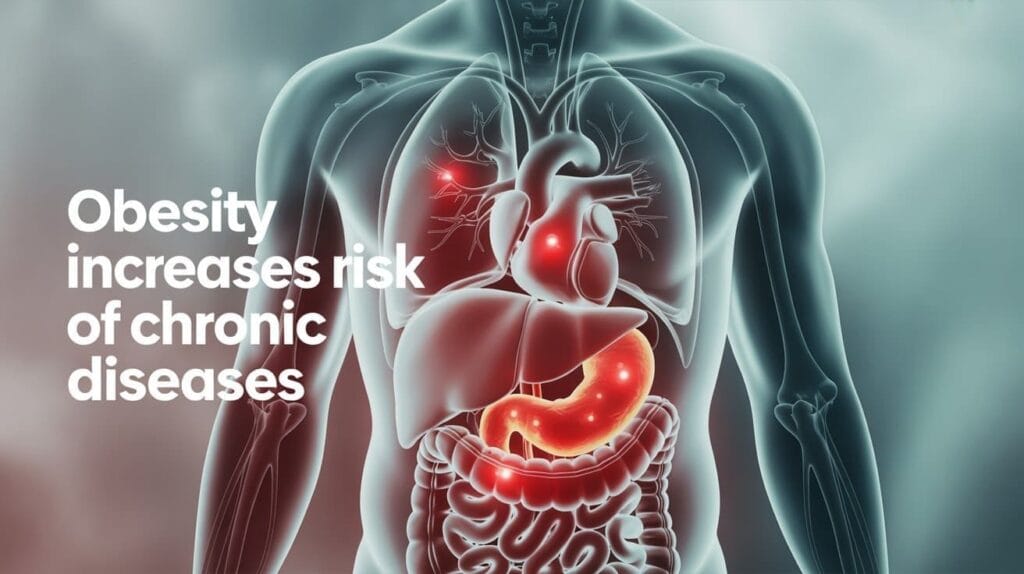
Health risks: What does the evidence show?
Excess body weight is a leading risk factor for noncommunicable diseases (NCDs). High-quality evidence from cardiovascular and population studies demonstrates that obesity increases the risk and severity of:
- Coronary heart disease, heart failure, and stroke
- Type 2 diabetes (strong and dose-dependent relationship)
- Certain cancers (breast, colorectal, endometrial)
- Musculoskeletal conditions (osteoarthritis, back pain)
- Sleep apnea, fatty liver disease, and reproductive disorders
The American Heart Association and major cardiovascular journals have published syntheses linking obesity to incident cardiovascular risk through pathways such as dyslipidemia, hypertension, insulin resistance, and systemic inflammation. AHA Journals+1
Recent notable studies and expert voices (Asia, America, Europe)
- Asia: Researchers analyzing regional trends and burdens (e.g., Zhou et al.) have quantified the rising contribution of high BMI to disability and mortality in East Asia and globally, emphasizing prevention and health system readiness. The Lancet
- America: Work by U.S. clinicians and public-health scientists (e.g., authors contributing to American Heart Association advisories) highlights the cardiovascular implications of obesity and practical clinical implementation strategies. AHA Journals+1
- Europe: Large consortiums led by European investigators and Lancet authors produced global prevalence and forecasting studies (e.g., the Lancet analyses that reported >1 billion people with obesity), providing the global epidemiologic context for policy action. Organisation mondiale de la santéThe Lancet
These studies reflect cross-continental collaboration and consistently call for multi-sector interventions—from individual clinical care to taxation and regulation of unhealthy foods—to bend the curve on obesity.

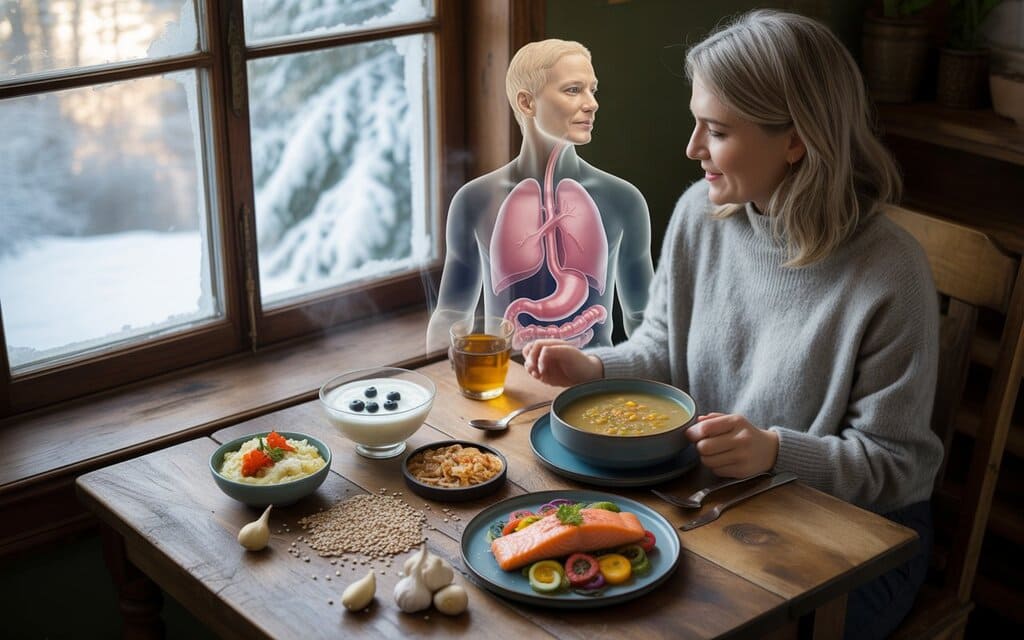
Evidence-based solutions : What works?
1. Nutritional interventions
- Emphasize whole foods, vegetables, fruits, legumes, lean proteins, whole grains, and unsaturated fats.
- Limit ultra-processed foods, added sugars, and sugary drinks. Systematic reviews of dietary patterns (including plant-based and sustainable diets) show metabolic benefits and potential long-term risk reduction when adopted at scale. PMC
2. Physical activity
- Aim for ≥150 minutes/week of moderate-intensity aerobic activity (or 75 min vigorous), plus resistance training twice weekly.
- Practical programs (walking, swimming, cycling, group exercise) reduce adiposity and improve cardiometabolic health.
3. Behavioral and psychological approaches
- Motivational interviewing, goal-setting, self-monitoring, and cognitive-behavioral strategies improve adherence.
- Addressing sleep, stress, and mental-health comorbidities supports sustainable change.
4. Medical and surgical treatments
- For patients with severe obesity or obesity with complications, pharmacotherapy (GLP-1 receptor agonists and other agents) and bariatric surgery are effective treatments that reduce weight and improve metabolic outcomes when indicated and supervised by specialists. Large clinical trials from multiple regions support these options as part of comprehensive care.
5. Population and policy measures
- Fiscal policies (sugar taxes), restrictions on junk-food marketing to children, improved food labeling, urban planning that encourages activity, and school-based nutrition programs are effective at scale. International health agencies recommend combining clinical care with public-health interventions. Organisation mondiale de la santénutrition.bmj.com
Practical plan (example) — A 12-week starter framework
| Week | Focus | Actions |
|---|---|---|
| 1–2 | Assessment & goal setting | BMI, waist, labs; set SMART goals |
| 3–6 | Nutrition baseline & activity ramp | Replace sugary drinks, 30 min walking ×5/week |
| 7–10 | Behavioral skills & intensity | Portion control, strength training twice weekly |
| 11–12 | Review & maintenance plan | Reassess, plan for relapse prevention |
Common myths and facts
- Myth: Obesity is just a lack of willpower.
Fact: Obesity is influenced by biological, environmental, social, and psychological factors—complex and treatable. The Lancet - Myth: All calories are the same.
Fact: Food quality affects satiety, metabolism, and long-term health beyond calorie counts.
Conclusion
Obesity and overweight are preventable and manageable conditions, but addressing them requires evidence-based personal care and bold public-health policies. Leading studies and expert groups from Asia, North America, and Europe converge on the need for integrated strategies: balanced nutrition, regular physical activity, behavioral support, and targeted medical interventions when necessary. Policymakers, clinicians, communities, and individuals each have a role to play. By combining clinical care with environmental and policy changes, we can reduce the burden of obesity, improve population health, and prevent the downstream consequences—cardiovascular disease, diabetes, and cancer—that follow excess adiposity. For practical help, consult a registered dietitian, exercise professional, or your healthcare provider to develop a personalized, safe plan.
Selected References & Further Reading
- World Health Organization — Obesity and Overweight (fact sheet). Organisation mondiale de la santé
- The Lancet — global analyses on obesity prevalence and trends (Lancet obesity collection; 2024–2025). The LancetOrganisation mondiale de la santé
- Powell-Wiley TM et al., Circulation / American Heart Association — Obesity and cardiovascular disease (scientific statement). AHA Journals+1
- Zhou XD et al., eClinicalMedicine/The Lancet — Burden of disease attributable to high BMI (2024). The Lancet
- Mambrini SP et al., systematic review on plant-based and sustainable diets (2025). PMC
- Global Burden of Disease project / Institute for Health Metrics and Evaluation — data and forecasts. healthdata.orgPMC