Introduction
Winter brings with it snow, chilly winds, and festive holidays — but it also brings increased risk of illness, cold and flu viruses, and common digestive disturbances. While many focus on wearing warm clothes and taking supplements, one critical yet often overlooked factor in maintaining robust health during winter is gut nutrition. The health of your digestive system directly influences your immune system, mood, energy levels, and overall well-being.
In recent years, scientific research across Asia, America, and Europe has highlighted the importance of gut microbiota — the complex ecosystem of microorganisms living in the digestive tract — in supporting immune function, inflammation control, and metabolic health (Turnbaugh et al., Nature, 2007; Thursby & Juge, Cellular and Molecular Life Sciences, 2017). A balanced gut helps the immune system identify harmful pathogens and mount an effective defense. Thus, gut nutrition in winter is not just about avoiding digestive discomfort — it plays a pivotal role in strong immunity and overall health.
This comprehensive article explores why winter gut nutrition matters, outlines key strategies and foods for gut health, presents a practical plan for daily nutrition, incorporates findings from medical research, and provides a clear roadmap to support your immune system this winter.
Key Points at a Glance
| Topic | Key Takeaway |
|---|---|
| Gut–Immune Connection | ≈70% of the immune system is linked with the gut lining and microbiota. |
| Winter Challenges | Cold weather changes eating patterns, lowers vitamin D, and impacts gut flora. |
| Nutrients for Gut Health | Dietary fiber, probiotics, prebiotics, and fermented foods are essential. |
| Foods to Avoid | Excess sugar, processed foods, and artificial additives hurt gut bacteria. |
| Hydration Matters | Adequate fluids support digestion and immune responses. |

Understanding the Gut–Immune System Connection
The gut and the immune system are deeply interconnected. Up to 70% of immune cells are located in gut-associated lymphoid tissue (GALT), which interacts closely with gut microbes to distinguish harmless substances from pathogens (Hooper et al., Science, 2012). This means that gut health is directly tied to immune resilience, particularly during winter when viral threats abound.
How the Gut Influences Immunity
- Barrier Function:
The gut lining acts as a physical barrier that prevents harmful organisms from entering the bloodstream. Poor nutrition can weaken this barrier — a phenomenon sometimes referred to as “leaky gut” — allowing toxins and bacteria to penetrate and trigger inflammation. - Microbiota Diversity:
A diverse gut microbiome supports balanced immune activity. Good bacteria help train immune cells, produce antimicrobial compounds, and reduce excessive inflammation. Overgrowth of harmful bacteria, on the other hand, can trigger immune dysregulation. - Inflammation Control:
Many immune disorders stem from chronic inflammation. Healthy gut microbes produce short-chain fatty acids (SCFAs), such as butyrate and acetate, which lower inflammation and support immune balance (Zhao et al., Annual Review of Food Science and Technology, 2019).
Winter Challenges to Gut Health and Immunity
During winter, several factors can negatively impact gut nutrition:
1. Reduced Sunlight and Vitamin D Levels
Limited sunlight exposure in winter decreases vitamin D synthesis. Vitamin D plays a role in immune regulation and maintaining the integrity of the gut lining (Martineau et al., The Lancet Diabetes & Endocrinology, 2017). Low levels are associated with greater susceptibility to respiratory infections.
2. Dietary Shifts
People often consume heavier, comfort foods in winter, including sweets, processed snacks, and high-fat meals. These can disrupt gut microbial balance, reducing beneficial bacteria and increasing inflammation.
3. Lower Hydration
Cold weather can reduce thirst sensation, leading to dehydration. Inadequate fluid intake slows digestion, increases constipation, and hampers nutrient absorption — all of which weaken immune function.
4. Stress and Sleep Disruption
Holiday stress and disrupted sleep can alter gut microbiota, further lowering immunity (Bested et al., Journal of Neuroimmune Pharmacology, 2013).

Core Nutrients and Foods for Winter Gut Nutrition
A . Dietary Fiber
Fiber feeds beneficial gut bacteria and increases the production of SCFAs. Good sources include:
- Whole grains (oats, barley, brown rice)
- Beans and lentils
- Vegetables (broccoli, carrots, brussels sprouts)
- Fruits (apples, pears)
- Nuts and seeds
Recommended Intake: At least 25–30 grams of fiber daily for adults.
B . Probiotics
Probiotics are live bacteria that support a healthy microbiome. They are especially beneficial during winter because they help maintain microbial balance.
Probiotic-rich foods include :
- Yogurt with live cultures
- Kefir
- Sauerkraut
- Kimchi
- Miso
- Tempeh
Clinical studies show that probiotics can reduce the duration of respiratory infections and promote immune responses (Hao et al., BMJ, 2015).
C . Prebiotics
Prebiotics are fibers that promote growth of beneficial bacteria. Key prebiotic-rich foods:
- Garlic
- Onions
- Leeks
- Jerusalem artichokes
- Asparagus
- Bananas
Prebiotics enhance gut microbiota diversity and improve immune signaling.
D . Healthy Fats (Omega-3 Fatty Acids)
Omega-3s reduce inflammation and support intestinal barrier integrity. They are found in:
- Fatty fish (salmon, mackerel, sardines)
- Walnuts
- Chia seeds
- Flaxseeds
Studies indicate that omega-3-rich diets reduce systemic inflammation and enhance immune defense (Calder, Nutrients, 2013).
E . Fermented Vegetables
Fermented foods add beneficial microbes and enhance nutrient absorption. Kimchi and sauerkraut are rich in vitamins C and K2, boosting immunity and supporting gut ecology.
Foods and Habits to Avoid for Better Gut Health
- High Sugar and Artificial Sweeteners
Excess sugar feeds harmful bacteria and promotes inflammation. - Highly Processed Foods
These foods lack prebiotic fiber and contain additives that negatively alter microbiota. - Excessive Alcohol
Alcohol irritates the gut lining and suppresses immune cells. - Frequent Antibiotic Use (without Medical Necessity)
Antibiotics disrupt microbiota diversity. When medically necessary, pair antibiotic treatment with a probiotic-rich diet.
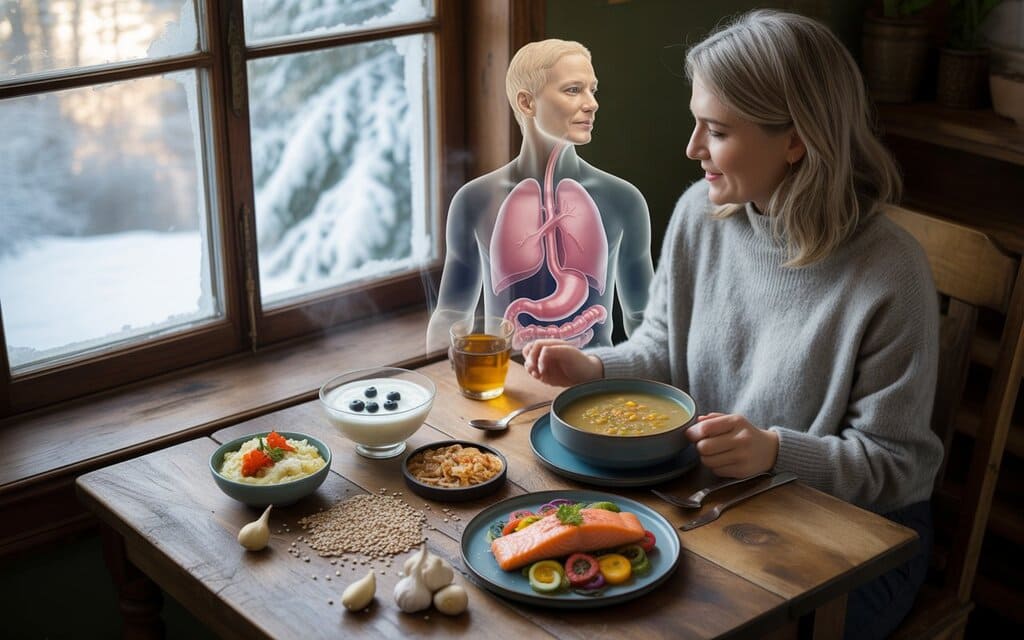
Building a Daily Winter Nutrition Plan for Gut Health
Here’s an example of a balanced winter day focused on gut nutrition and strong immunity.
Breakfast
- Overnight oats with chia seeds, berries, and a spoonful of kefir
- Green tea or warm lemon water
Why it works : Oats and chia seeds provide fiber; kefir adds probiotics.
Mid-morning Snack
- Apple slices with almond butter
Why it works: Apples offer fiber and antioxidants; almonds add healthy fats.
Lunch
- Warm lentil soup with carrots, garlic, and onions
- Side of kimchi or sauerkraut
Why it works : Lentils are rich in fiber and protein; garlic and onions are prebiotic sources; kimchi adds probiotics.
Afternoon Snack
- Yogurt with honey and walnuts
Why it works : Yogurt boosts beneficial bacteria; walnuts provide omega-3 fats.
Dinner
- Baked salmon with roasted Brussels sprouts and brown rice
Why it works : Omega-3s support anti-inflammatory pathways; sprouts and brown rice add fiber.
Before Bed
- Herbal tea (e.g., ginger, peppermint)
Why it works : Calms digestion and supports restful sleep.
Hydration and Movement : The Unsung Heroes
Hydration
Even in winter, drinking water is vital. Aim for 8–10 cups of fluids daily, including herbal teas and water-rich soups. Proper hydration keeps digestion efficient and supports nutrient transport.
Physical Activity
Moderate physical activity — even brisk walking or gentle yoga — supports gut motility, reduces stress, and enhances immune function. Aim for at least 150 minutes of moderate exercise per week.
Recent Scientific Insights
Here are some leading studies highlighting the gut–immune connection:
- Microbiome Diversity and Immunity : Reduced gut microbiota diversity is linked with increased inflammation and susceptibility to infection (Zhao et al., Annual Review of Food Science and Technology, 2019).
- Probiotic Support for Respiratory Health : Randomized controlled trials show that specific probiotics can decrease the incidence and duration of respiratory infections in adults and children (Hao et al., BMJ, 2015).
- Vitamin D and Immune Regulation : A meta-analysis shows that optimizing vitamin D levels may reduce the risk of acute respiratory infections (Martineau et al., The Lancet Diabetes & Endocrinology, 2017).
- SCFAs and Immune Tolerance : Short-chain fatty acids produced by gut bacteria play a powerful role in reducing inflammatory responses and enhancing immune tolerance (Smith et al., Science, 2013).
Practical Tips to Reinforce Gut Health in Winter
- Start meals with fiber-rich foods
This supports fullness and feeds beneficial bacteria. - Include fermented foods daily
Even small servings contribute microbes that enrich your gut ecosystem. - Keep a food and symptom diary
Track how different foods affect your digestion, energy, and immunity. - Monitor vitamin D levels
Consider safe supplementation during winter months — particularly if sunlight exposure is low. - Prioritize sleep
Adequate sleep (7–9 hours) supports immune signaling and gut balance.
Conclusion
Winter need not be a season of weakened immunity, fatigue, or digestive discomfort. By prioritizing gut nutrition, you empower your body’s largest immune organ and cultivate resilience against common winter stressors. A diet rich in fiber, probiotics, prebiotics, omega-3s, combined with hydration, moderate exercise, and healthy lifestyle habits, strengthens your gut microbiome and enhances your overall health.
Whether you’re combating seasonal changes, supporting immunity, or improving digestion, the road to better health begins in the gut. This winter, let your nutritional choices be a source of strength — energizing your body, protecting your immune system, and enhancing your vitality through every cold season day.
Bibliography
- Turnbaugh, P. J., et al. (2007). The Human Microbiome Project. Nature, 449(7164), 804–810.
- Thursby, E., & Juge, N. (2017). Introduction to the Human Gut Microbiota. Cellular and Molecular Life Sciences, 74(2), 3177–3207.
- Hooper, L. V., et al. (2012). Interactions Between the Microbiota and the Immune System. Science, 336(6086), 1268–1273.
- Zhao, L. (2019). The Gut Microbiota and Obesity: From Correlation to Causality. Annual Review of Food Science and Technology, 10, 9.1–9.21.
- Hao, Q., et al. (2015). Probiotics for Preventing Acute Upper Respiratory Tract Infections. BMJ, 350, h1606.
- Martineau, A. R., et al. (2017). Vitamin D Supplementation to Prevent Acute Respiratory Infections. The Lancet Diabetes & Endocrinology, 5(6), 431–440.
- Calder, P. C. (2013). Omega-3 Polyunsaturated Fatty Acids and Inflammatory Processes. Nutrients, 5(2), 437–461.
- Smith, P. M., et al. (2013). The Microbial Metabolites, Short-Chain Fatty Acids, Regulate Colonic T Regulatory Cell Homeostasis. Science, 341(6145), 569–573.
- Bested, A. C., et al. (2013). Gut Microbiota, Immunity, and Central Nervous System. Journal of Neuroimmune Pharmacology, 8(4), 651–670.
- Wikipedia contributors. (n.d.). Gut Microbiota — Wikipedia, The Free Encyclopedia. (Access date 2026).





