Introduction
As temperatures soar during the summer months, managing chronic health conditions becomes more challenging—especially for individuals living with diabetes mellitus. Heat and humidity can disrupt blood sugar levels, increase the risk of dehydration, and interfere with medications and insulin storage. According to the Centers for Disease Control and Prevention (CDC), over 38 million Americans have diabetes, and many are unaware of the added health risks they face in summer.
In this comprehensive article, we will explore how summer heat impacts diabetic patients, the physiological risks involved, and evidence-based preventive measures. We’ll also examine recent medical studies and include a visual chart summarizing key recommendations.

Understanding Diabetes and the Summer Heat
Diabetes is a chronic metabolic disorder that impairs the body’s ability to produce or effectively use insulin, a hormone responsible for regulating blood glucose levels. There are two main types of diabetes:
- Type 1 Diabetes: An autoimmune condition where the pancreas produces little or no insulin.
- Type 2 Diabetes: A lifestyle-related condition characterized by insulin resistance.
Why Summer Is Risky for Diabetics
People with diabetes are at increased risk in hot weather for several reasons:
- Dehydration: High temperatures increase fluid loss through sweating, leading to elevated blood glucose levels.
- Hypoglycemia: Heat can increase insulin absorption, especially with physical activity, potentially causing dangerously low blood sugar.
- Medication Instability: Insulin and some diabetes medications lose their effectiveness when exposed to heat.
- Heat Sensitivity: People with diabetic neuropathy may have reduced ability to feel temperature changes, putting them at greater risk of heat-related illness.
A 2021 study published in Diabetes Care found that “the incidence of heat exhaustion and hospitalization among diabetics increased by 14% during summer heatwaves” compared to cooler months.
Key Summer Risks for Diabetics
1. Dehydration and Electrolyte Imbalance
One of the primary summer concerns is dehydration. High temperatures cause the body to sweat more, leading to fluid and electrolyte loss. For diabetics, this can result in elevated blood sugar levels as the body’s glucose becomes more concentrated in the bloodstream.
Tip: Drink water regularly even if you’re not thirsty. Avoid sugary beverages and limit caffeine, which can worsen dehydration.
2. Blood Sugar Fluctuations
Heat can make it harder to control blood sugar levels. Insulin absorption can accelerate, particularly when injected near active muscles (e.g., arms or legs during outdoor exercise), which increases the risk of hypoglycemia.
Key Signs of Hypoglycemia:
- Dizziness
- Sweating
- Confusion
- Weakness
- Irritability
3. Insulin Storage Issues
Insulin must be kept between 36°F and 46°F (2°C to 8°C). If exposed to heat, it may degrade, leading to uncontrolled blood sugar.
According to WebMD, “Insulin becomes unstable when exposed to temperatures above 86°F (30°C) for extended periods.”

4. Foot Infections and Skin Conditions
Sweat, friction, and high humidity can cause fungal infections, blisters, and ulcers, especially in diabetic patients with neuropathy. Walking barefoot at the beach or pool also increases the risk of foot injuries.
The American Diabetes Association warns that “small foot wounds may go unnoticed in diabetic neuropathy, leading to serious infections.”
Preventive Measures for Diabetic Patients in Summer
To enjoy a safe and healthy summer, diabetic individuals must take proactive steps. Below are essential preventive strategies:
1. Stay Hydrated
- Carry a water bottle at all times.
- Drink at least 2–3 liters of fluids per day, adjusting for activity and weather.
- Add electrolyte solutions if needed.
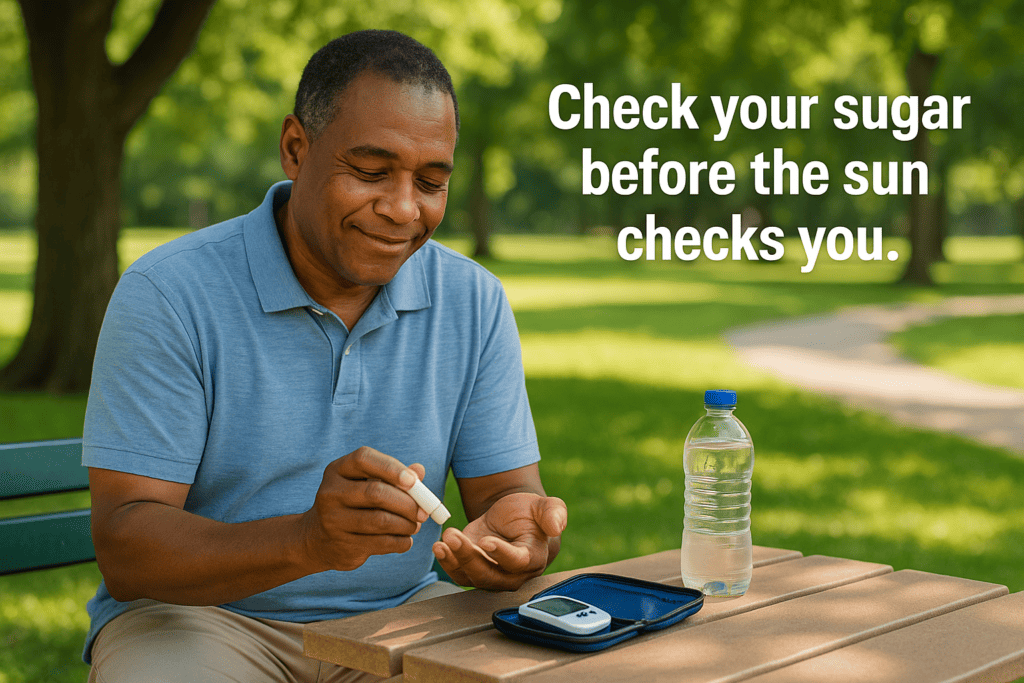
2. Monitor Blood Glucose Frequently
- Check blood sugar levels more often than usual.
- Keep a log of readings during exercise or outdoor activities.
- Always have a fast-acting carbohydrate snack (e.g., glucose tablets, juice).

3. Store Medications Properly
- Use a cool pack or insulated bag for insulin while traveling.
- Never leave insulin or testing equipment in a hot car.
- Use a digital thermometer to monitor insulin storage temperature.
4. Dress Appropriately
- Choose light-colored, breathable fabrics (e.g., cotton or moisture-wicking material).
- Wear protective footwear to avoid blisters and burns.
- Use sunscreen with SPF 30 or higher to protect skin, especially if using photosensitive medications.
5. Avoid Peak Heat Hours
- Limit outdoor activities between 10 a.m. and 4 p.m.
- Schedule walks or exercise in the early morning or evening.
6. Recognize Early Warning Signs
Be aware of signs of heat exhaustion or hypoglycemia. Early symptoms include:
- Excessive sweating or lack of sweating
- Muscle cramps
- Headache or nausea
- Confusion or fatigue
7. Consult Your Healthcare Provider
- Review your medication regimen for heat sensitivity.
- Discuss any dose adjustments for insulin or other drugs.
- Consider a summer-specific diabetes management plan.
Chart: Summer Diabetes Risks & Protective Actions
| Risk | Effect on Diabetics | Recommended Action |
|---|---|---|
| High temperatures | Increases dehydration and glucose levels | Drink water regularly, stay indoors during peak heat |
| Sun exposure | Skin damage, risk of foot burns | Wear sunscreen and protective clothing |
| Insulin degradation | Poor glucose control | Store insulin in a cool pack |
| Hypoglycemia during activity | Confusion, fainting | Monitor glucose and carry glucose snacks |
| Infections (foot, skin) | Wounds may not heal quickly | Inspect feet daily, wear clean socks and shoes |
Medical Studies and Expert Opinions
- A 2022 study in the Journal of Clinical Endocrinology & Metabolism confirmed that diabetics are twice as likely to suffer from heatstroke compared to non-diabetics.
- According to the National Institutes of Health (NIH), “diabetics must take additional precautions during summer months, especially in regions with heatwaves, to prevent metabolic complications.”
- Dr. Anne Peters, a renowned endocrinologist at Keck School of Medicine, recommends diabetics “carry a glucose meter and water bottle at all times during summer trips or outings.”
For additional reading:
Conclusion
Summer heat presents unique risks for individuals living with diabetes, including dehydration, fluctuating blood sugar levels, and insulin instability. These dangers can be mitigated through awareness, preparation, and proactive care. From hydration strategies to medication management, a thoughtful summer plan can help diabetic patients enjoy the season safely.
Remember to monitor blood glucose regularly, stay cool and hydrated, and consult your doctor for personalized advice. With these measures, you can maintain your health and well-being even during the hottest months of the year.